Crack is back – so how dangerous is it and why is its use on the up?
Ian Hamilton, University of York; Harry Sumnall, Liverpool John Moores University, and Mark Monaghan, Loughborough University
There have long been scare stories about drugs so we need to be careful when interpreting new drug use data. But recent reports suggest that crack cocaine use is on the rise again.
Crack emerged in the Americas in the late 1970s as a relatively cheap and transportable form of cocaine that could be more easily distributed than the powdered variety and soon led to what was widely described as an “epidemic”, especially in the US.
Supporters of drug reform in the US have long highlighted the uneven application of the law concerning crack and powder cocaine. Referred to as the “100-1 Rule”, until the passing of the 2010 Fair Sentencing Act, possession of one gram of crack in America was treated as the equivalent of 100g of powder cocaine. As crack use was associated with the black, urban poor and powder cocaine with the more affluent white middle classes, this policy became symbolic of the racism of the “war on drugs” and the over-representation of black men in the US prison system .
By the late 1980s, crack was also being used in the UK, and in 2002 the British government was concerned enough to produce a national crack strategy. And now, after a relative reduction in use, the drug is making a worrying comeback.
What is crack?
The physical and psychological effects of crack are similar to powdered cocaine – usually cocaine hydrochloride, which is mainly administered through the nostril as a powder. In chemical terms, crack is the free base (non-salt based) form of cocaine, which makes it volatile enough to be inhaled through smoking, although more people in England and Wales are now injecting it.
Both forms of cocaine act as a stimulant and produce similar “highs”. But what makes crack more potent than powder cocaine is the immediacy, duration, and magnitude of its effect, as well as the typical frequency and amount used. There are concerns over the long-term effects of cocaine in all its forms, and it has been associated with neurological and neuropsychiatric changes, as well as damage to the heart and lungs.
The risk of dependence among users of crack cocaine has also been estimated to be two to three times greater than among powder cocaine users.

Price and availability
Beyond wider drug trends and fashions, price, purity and availability are considered to be important drivers of drug use over time. Not only has the price of crack fallen by 13% since 2007 but it is now more readily available. Newly established supply routes in the UK have also emerged. Central city gangs distribute crack into coastal and rural areas, along so-called “county lines”. The Home Office reports that the number of seizures of crack in Britain are currently at their highest since 2008, although the weight of seizures has fallen since 2015-16.
Household surveys typically underestimate the use of drugs such as heroin or crack, but statistical modelling suggests that the number of people using crack in England has increased by 10%, with 166,640 users in 2010-11 rising to 182,828 by 2014-15.
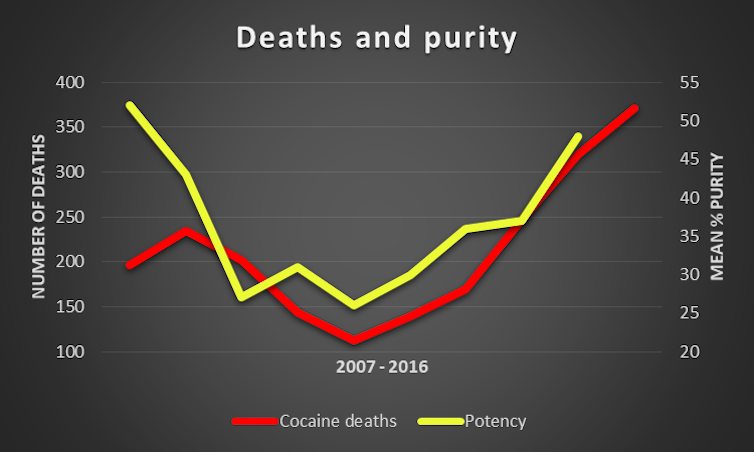
These trends in price, availability and use have also been accompanied by crack becoming increasingly pure. And that could be having an effect on the number of fatalities caused by it.
Crack is rarely recorded as contributing to death by coroners, as toxicological assessments don’t distinguish between the different forms of cocaine. But cocaine deaths in England and Wales rose from 320 in 2015 to 371 in 2016. The Office for National Statistics (ONS) commented that there was a significant increase in both crack and powder cocaine purity at all levels in 2016, which may partly explain this increase.
Treatment
Another trend suggesting crack use is on the rise is data on treatment presentations. The average age of a person using crack cocaine presenting to treatment is 35. But this year has seen a 30% rise in young people under the age of 25 accessing treatment for problems with crack. It is a decade since we witnessed a rise in this age group seeking help for crack.
Additionally, unlike effective opioid agonist therapies, such as methadone for heroin use, there is no substitute drug that can be given to those seeking to stabilise and reduce crack use. Around 41% of people presenting to treatment services in England and Wales also report using both opioids and crack, which can present additional challenges.
Overall, reviews of evidence suggest that psychosocial interventions (behavioural and “talking” therapies) for cocaine users can keep people in contact with treatment services, but do not necessarily lead to a reduction in (crack) cocaine use. One approach, called contingency management, which provides a system of incentives (such as vouchers, employment, or loosening clinic attendance requirements) to make abstinence more attractive than continued drug use shows promise, but there are some remaining questions about the longevity of the treatment’s effect.
Anecdotally, some people trying to reduce their use of crack have reported that cannabis has helped. However, there is only limited scientific evidence to support this, and so more research is required.
Why is crack back?
As various ethnographic studies have shown, crack has been part of the urban landscape for decades. With high levels of youth unemployment alongside cuts to social and other services under austerity, participation in illicit economies becomes one of the only income generating opportunities available for those who would otherwise have to negotiate life on a low income. After all, inequality between the rich and poor, has been show adversely to impact people who are dependent on drugs.
Ian Hamilton, Lecturer in mental health and addiction, University of York; Harry Sumnall, Professor in Substance Use, Liverpool John Moores University, and Mark Monaghan, Lecturer in Crimimology and Social Policy, Loughborough University
This article was originally published on The Conversation. Read the original article.
Comments
Post a Comment